Insurance denied an $800,000 seizure drug — twice. A state-run panel helped a teen get it.
NegativeHealth
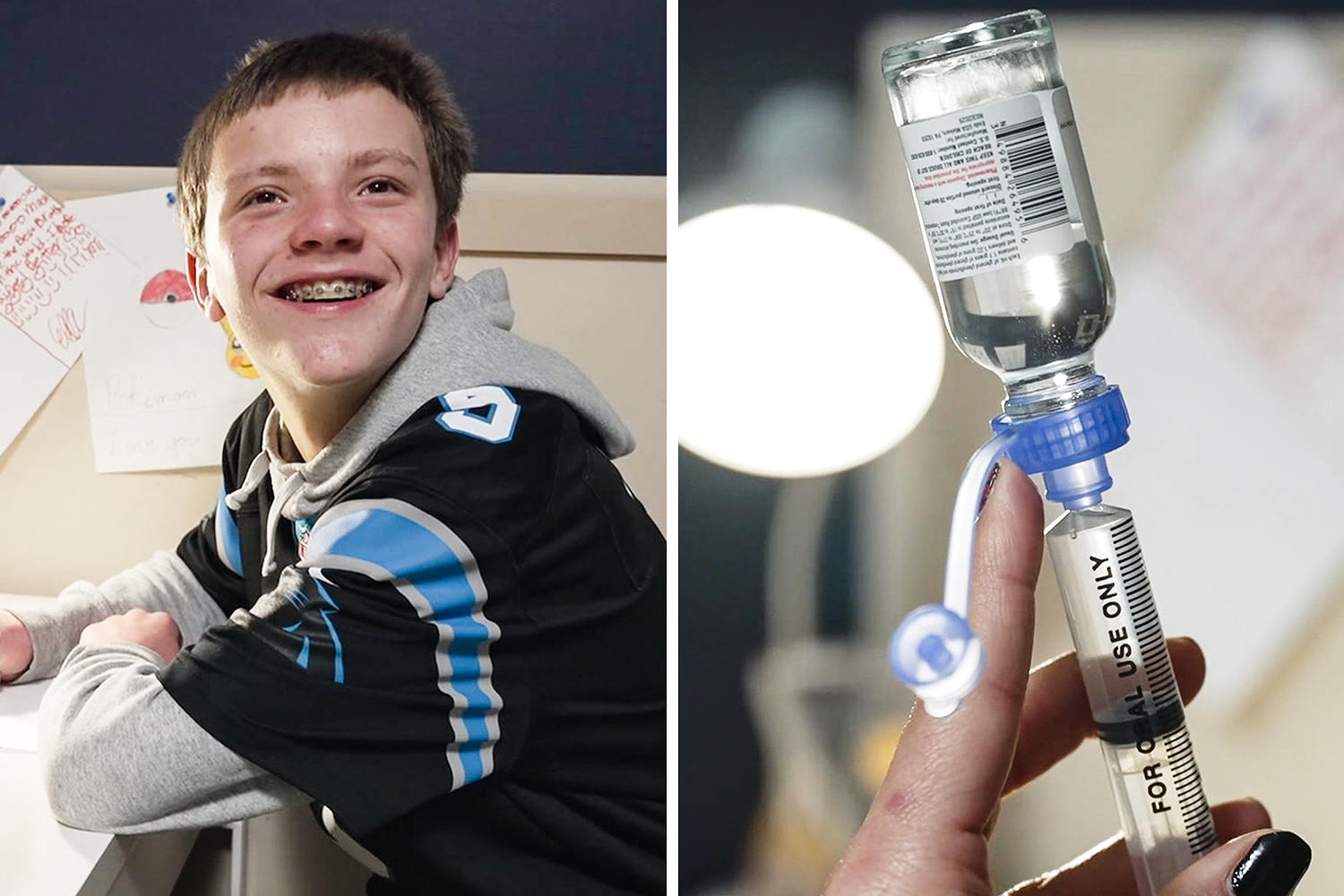
- Paxton Pope, a teenager suffering from frequent seizures, faced significant challenges when his insurance denied coverage for a nearly $800,000-a-year medication that his doctor believed could greatly reduce his condition. After two refusals, a state-run panel intervened to help secure the necessary treatment for him.
- This development is crucial for Paxton and his family as it not only alleviates immediate financial burdens but also provides hope for improved health outcomes. Access to such expensive medications can be life-changing for patients with severe medical conditions.
- The situation underscores a broader issue within the healthcare system, where families often struggle to obtain necessary treatments due to insurance denials. Similar cases, such as a mother advocating for her daughter's scoliosis surgery, highlight the ongoing challenges many face in navigating insurance policies and securing essential medical care.
— via World Pulse Now AI Editorial System




